The Six Fracture Modes of Teeth – Graeme Milicich – The British Dental Conference and Dentistry Show 2019
Featured Products Promotional FeaturesPosted by: Dental Design 19th March 2019
The Six Fracture Modes of Teeth
G W Milicich BDS

Teeth fracture for several reasons. It is very uncommon for a sound tooth to fail, but once a tooth has had a restoration placed, fractures begin to develop over a period of time. When we look very closely at how Mother Nature designed our teeth, several biomechanical strategies have been employed to ensure they can function for many decades. However, our modern diet and the associated decay epidemic, along with the required invasive management of the resultant decay disturbs the complex stress distribution system within a tooth. Effectively, a tooth behaves like a compression dome, similar to a cathedral dome. The enamel Bio-dome is designed to keep the underlying dentine in compression. When the enamel cap is disturbed to restore a tooth, important structures are damaged and this exposes the underlying dentine to tensile stresses it was not designed to cope with.
There are several structures within enamel that work in strain harmony to ensure stability of the tooth. These include the sub-occlusal oblique transverse ridge, Rainey’s Web, the peripheral rim of enamel, occlusal enamel in general, and the Bio-rim (cervical half of the tooth). From a dentistry perspective, we should ideally be retaining these structures when restoring teeth. To achieve this, our primary gaol is to ensure retention and stability of the occlusal surface of the tooth. Minimally invasive dentistry’s primary aims are to manage a pathogenic biofilm and train it back to health. However, this is not always achievable, so protecting the fissure complex from damage is very important. This relies on being able to diagnose a pathogenic biofilm, or the early demineralization within a fissure complex, utilising all the modern technology we now have available, and predictably seal the fissures with autocure GIC. However, once the occlusal integrity has been disrupted, concentrated stresses within the underlying dentine lead to crack propagation and eventual failure of tooth structure. We must recognise enamel is not homogeneous, it is a very complex anisotropic structure, with amazingly subtle variations in ultrastructure and prism orientation, depending on the loads that have to be dissipated.
There are six basic fracture modes within teeth.
The first two are associated with fractures in the peripheral rim of enamel.
Figure 1

Figure 2
- The first is described as “occlusal effect decay”. Once the occlusal enamel is cut, compression on a working cusp can cause distortion in the peripheral rim of enamel. This leads to an unstable vertical fracture where decay first become established at the EDJ and then work into the dentine and outwards to the surface of the enamel, following the internal walls of the vertical fracture. This fracture mode does not have an underlying dentine fracture.
Figure 3

- The second is a delamination of occlusal enamel and peripheral rim enamel beside an amalgam. Once again, the loss of the occlusal enamel allows the peripheral rim to flex under compressive forces, primarily on the working cusps. Investigating the complexities of the enamel cap, there is a distinct defining interface between occlusal and peripheral rim enamel that will delaminate if the peripheral rim enamel is flexing due to lack of support from the occlusal enamel. The adjacent amalgam provides no support to the surrounding enamel.
Figure 4

- Oblique cusp fractures. This is the most common fracture presentation that we see on a daily basis in our practices. Placing an amalgam into the occlusal of a tooth, that may or may not include either or both of the interproximal surfaces, exposes the underlying cuspal dentine to tensile forces. Over a period of years, a crack begins to propagate, eventually leading to the cusp fracturing off.
Figure 5

Figure 6

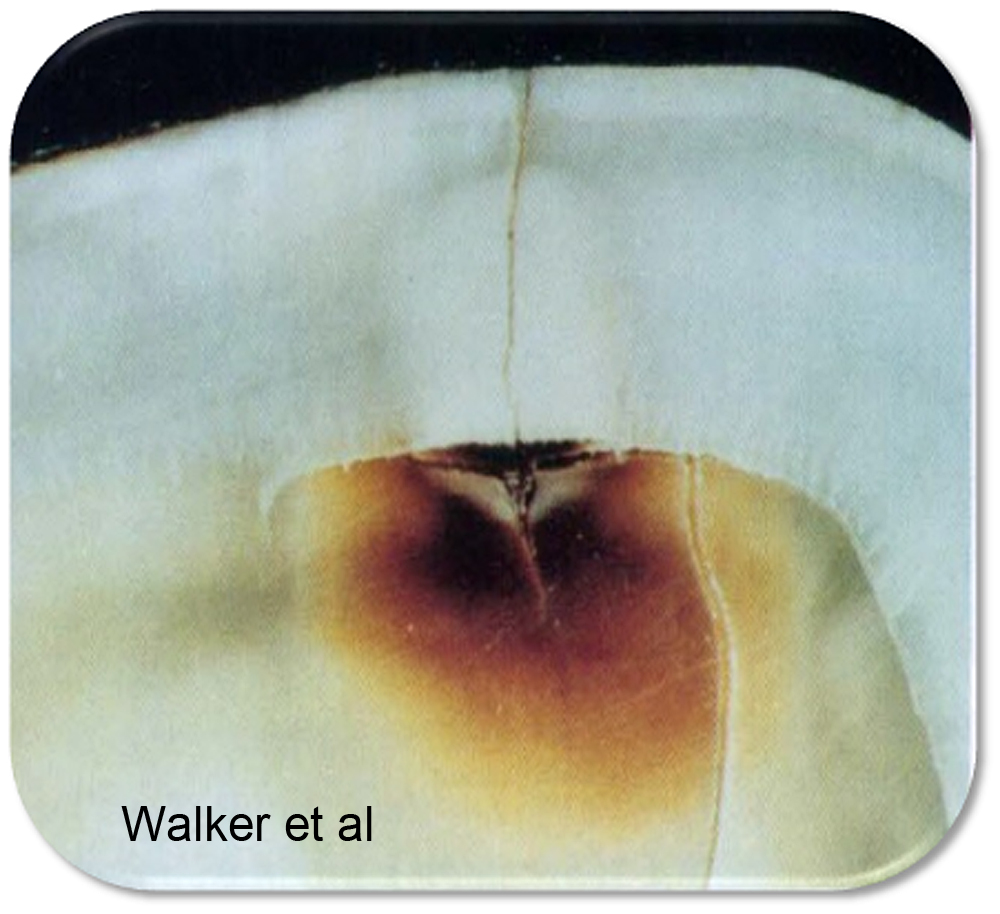
Even though there is “only” an occlusal amalgam, this tooth has developed a mesio-distal fracture, as well as Poisson Effect fractures in the dentine underlying the amalgam.
- Mesio-distal fractures. This fracture mode is the nightmare of dentistry. Often diagnosis is difficult and symptoms are vague. This fracture mode is driven by vertical loads driving adjacent cusps apart, placing the underlying dentine into tension, but rather than the fracture generating obliquely, it travels vertically towards the pulp. Correct diagnosis and intervention can save most of these teeth.
(This tooth had all 4 cusps fail due to oblique fractures, but it also had multiple Poisson effect fractures)
- Poisson Effect Fracturing. A recently identified fracture mode that occurs under old amalgams. Once again, when the occlusal enamel is disrupted, the underlying dentine is exposed to tensile forces. Dentine is compressible and as a consequence is exposed to Poisson distortion. This can best be visualised as barrel distortion of the tooth. The overlying amalgam acts as a force concentrator, compressing the underlying dentine that then goes into radial tension. This leads to micro-fracturing of the dentine, creating random, often disconnected spiderweb-like fractures in the floor of the cavity. These can be present even in teeth with oblique or vertical fractures.
- Traumatic fractures. These are generally associated with either an external blow or an unexpected foreign object in food.
It is important that the fracture modality is accurately identified because management is quite varied. The primary goal is to identify where the forces that are causing the damage being applied to the tooth. If a crack is not dealt with correctly, the tooth can continue to exhibit symptoms and often a secondary diagnosis of an irreversible pulpitis is made, leading to unnecessary endodontics. If the fracture is correctly diagnosed and treated, the tooth generally settles.
As an overview, the goal is to re-create a stable compression dome to prevent the underlying dentine from being exposed to tensile forces. With more damaged teeth, this is best achieved with an adhesive ceramic onlay. However, depending on the fracture type, many teeth can be predictably stabilised using direct bonded composite in conjunction with Ribbond fibre reinforcing. Success relies on being able to predictably bond to tooth structure in the long term. Some in our profession do not believe this is possible, but clinical success for over 30 years using the Biomimetic techniques described in my lecture in the BDA Theatre will prove it is not only possible, but totally predictable. Once we come to an understanding of how a tooth functions at a biomechanical level, it becomes easier to diagnose the various failure modes of teeth and then predictably restore them. Equally, the less you do to a tooth in the beginning, the less you will have to do to it in the future.
When a minimally invasive philosophy is adopted, and biomimetic restorations become an option, dentists notice a significant change in their practices. The incidence of post treatment endodontics is reported by Biomimetic dentists to reduce by 80-90%, because they are diagnosing fractures accurately and treating them appropriately.
Dr Graeme Milicich will be discussing the topic in further detail within the BDA Theatre at the British Dental Conference and Dentistry Show 2019. Register for your free delegate pass to make sure you don’t miss out.
The British Dental Conference and Dentistry Show 2019 will be held on Friday 17thand Saturday 18thMay at the Birmingham NEC, co-located with DTS.
Visit www.thedentistryshow.co.uk, call 020 7348 5270
or email dentistry@closerstillmedia.com
Author biography:
Graeme Milicich
Graeme is a graduate of the University of Otago (Dunedin, NZ) and maintained a private general practice in Hamilton since 1977 (NZ) until 2017 when he retired from active practice. Throughout his career he developed a keen interest in the area of minimal intervention dentistry (MID), which was considered in decades past to be revolutionary. This area of interest quickly drew his attention to caries risk management, biomechanics and biomimetics as it applied to restorative dentistry – lasers and CAD/ CAM and their applications in minimally invasive dentistry have been at the forefront of Graeme’s expansion of MID concepts.
He has several peer-reviewed published articles and has presented at a national and international level in the field of MID, been recognised by several international bodies dedicated to furthering MID and laser dentistry and has been a clinical educator in CAD/CAM dentistry. Graeme has developed many training resources in the field of MID and undertaken clinical studies into the application of lasers for restorative dentistry.
No Comments
No comments yet.
Sorry, the comment form is closed at this time.